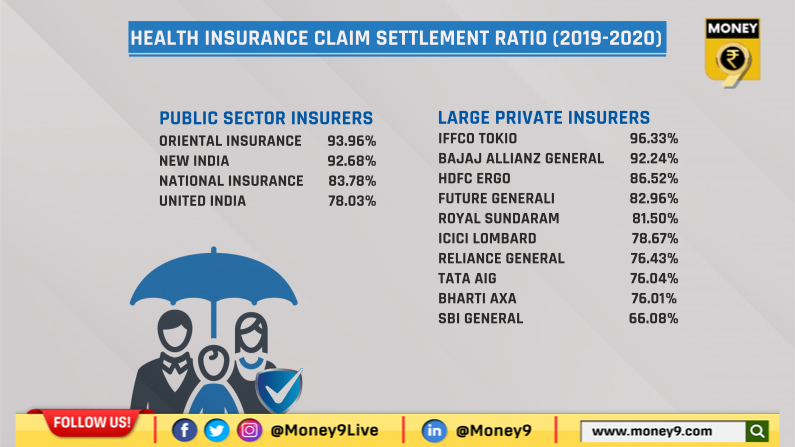
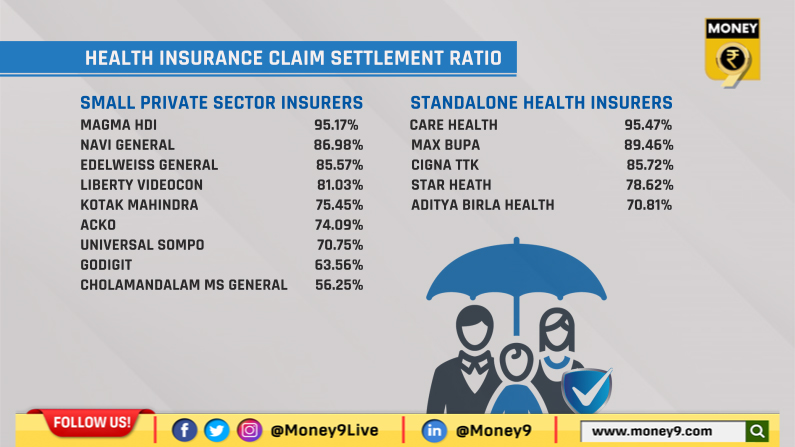
These health insurers have the best claim settlement ratio. Read on...
Among public sector insurers Oriental Insurance has the highest ratio at 93.96%.

One of the first things to check before buy a health insurance policy is the claim settlement ratio of the insurer. It is an indicator of the kind of services offered by an insurer during the time of emergency. Claim settlement ratio is calculated by dividing total number of claims settled in a year with the total number of claims available for processing during the year.
Insurance Regulatory and Development Authority of India (IRDAI) has recently put out data on claims which shows that IFFCO Tokio General Insurance has the highest claim ratio at 96.33%. Among public sector insurers Oriental Insurance has the highest ratio at 93.96% followed by New India, National Insurance and United India at 92.68%, 83.78% and 78.03% respectively. Bajaj Allianz is the second highest among private insures at 92.24%.
Source: IBAI
According to the annual report “During 2019-20, General and Health Insurers have settled 1.67 crore health insurance claims and paid Rs 40,026 crore towards settlement of health insurance claims. The average amount paid per claim was Rs 23,866. In terms of number of claims settled, 70 per cent of the claims were settled through TPAs and the balance 30 per cent of the claims were settled through in-house mechanism.”
In terms of mode of settlement of claims, 56 per cent of total number of claims paid were settled through cashless mode and another 40 per cent of the claims were settled through reimbursement mode. Insurers have settled 4 per cent of their claims amount through “both cashless and reimbursement mode”.
Source: IBAI
For a claim on cashless basis the treatment has to be done in a network hospital. Here the insurance company directly pays to the insurer and you don’t have to wait for reimbursement. If you get treatment in non-network hospital then you have to pay from your pocket and later make a claim from insurance company. There is generally of period of 7 to 15 days after the discharge during which you have to make a claim.
Experts say that during many months of lock down or partial lock down insurance industry benefitted as claims for hospitalization for normal treatments, surgeries even cancer treatment, accidental treatments have been much less. These numbers will be reflected in the next year annual report of IRDAI.

